This report explores the transformative impact of artificial intelligence (AI) on healthcare, focusing on its integration with big data for advanced diagnostics and treatment. AI-driven decision-support systems reshape medical methodologies, enabling early cancer detection and personalised care. While recognising the complementary nature of AI and human expertise in achieving comprehensive and effective healthcare outcomes, this report delves into groundbreaking studies leveraging machine learning and deep learning in cancer diagnosis. Ethical considerations highlight the importance of unbiased algorithms and addressing healthcare disparities. This report concludes by emphasising AI’s potential for equitable, accessible, and advanced medical solutions, marking a paradigm shift in healthcare.
AI’s Potential in Medicine: A Glimpse into the Future of Healthcare
Artificial Intelligence and Healthcare | Sanchani Brabhaharan
The rapid evolution of generative artificial intelligence (AI) and the growing use of big data is transforming healthcare and scientific exploration. Notably, healthcare facilities are progressively integrating AI-driven decision-support systems, fundamentally reshaping the landscape of diagnostic and treatment methodologies. Advancements now enable us to rapidly detect cancer, foresee diseases before they manifest, and identify potential genetic disorders that could affect us in the future. As this powerful tool becomes integrated into the health sector, it is crucial to understand its benefits to foster positive advancements.
In some cases, AI may take over scientific thinking, medical diagnoses, and surgeries. However, every individual and every case is different; therefore, the knowledge, care, and understanding that doctors have will continue to save many lives. Medical professionals can use AI to research, conduct tests, and efficiently predict and diagnose diseases, utilising the algorithm models created with massive datasets. For example, it is tough to run tests, and with a lack of hospital staff and time, it is challenging to carry out intraoperative histopathology to deliver rapid, accurate diagnostic images that inform decisions during surgery. On this front, AI can increase efficiency with a trained dataset for accuracy [1]. Can AI effectively drive other healthcare advancements into the future?
AI in Medicine: Earlier Cancer Detection?
Cancer continues to pose significant challenges to healthcare systems. Although interventions targeting the uncontrollable growth of these cancer cells have shown improvement in recent years, diagnosis at advanced stages, rather than early detection, compromises treatment outcomes and renders intervention strategies less effective. In this instance, AI emerges as an innovative approach to overcome the limitations inherent in the current diagnostic methodologies and interventions.
Machine learning (ML) is a form of AI where computers are designed to learn from data structures and algorithms to analyse and identify patterns. This can allow the technology to forecast and make informed predictions and decisions based on unseen data. ML can assist in a broad scope of medical research and clinical areas, particularly in predicting various types of cancer. Numerous studies and practices have indicated that integrating AI and ML has exhibited a higher accuracy in predicting cancer compared to traditional clinical assessments [2]. The significance of AI in healthcare lies in its ability to assimilate multifaceted data from diverse patient assessments, allowing for a personalised and precise approach to care, patient survival, prognosis, and disease progression predictions [2]. This advancement facilitates individualised care strategies unique to the conditions of each patient.
Study 1:
Research was undertaken to determine if ML could provide accurate diagnostic predictions for brain tumour specimens [1]. It explores the ability of ML to accurately classify stimulated Raman histology (SRH) images of fresh human brain tumour specimens. SRH is an imaging technique paired with ML and deep learning that helps to detect brain tumours automatically during surgery. The research involved developing a clinical SRH microscope, comparing SRH with traditional hematoxylin and eosin (H&E) images, and employing a multilayer perceptron (MLP) machine learning model. The results demonstrated that ML algorithms, particularly MLP, can effectively diagnose and detect brain tumours, showcasing the potential of combining ML with imaging techniques like SRH in medical applications.
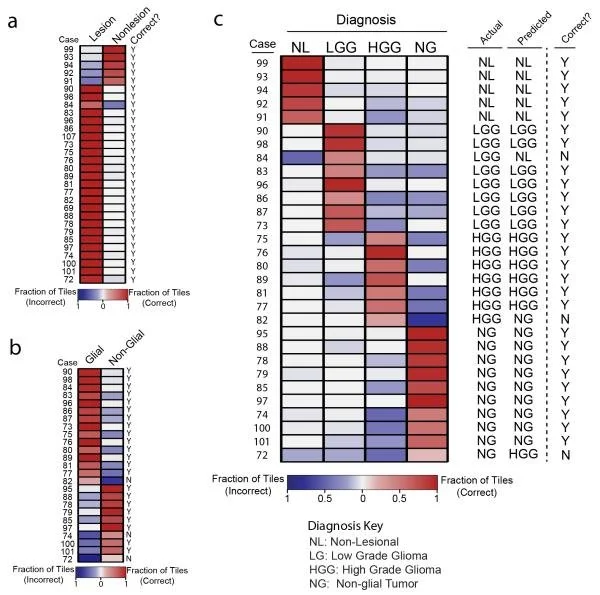
The accuracy of the MLP was rigorously tested using a leave-one-out approach, optimising the training set’s size while mitigating potential correlations between samples in both the training and test sets. This approach was applied to 30 cases, each falling into one of four diagnostic categories: non-lesional, low-grade glial, high-grade glial, or non-glial tumours, encompassing meningioma, lymphoma, metastases, and medulloblastoma. These categories were selected due to their critical significance in providing essential information to guide decision-making in brain tumour surgery. Figure 1 shows the level of prediction accuracy by utilising MLP, i.e., the machine learning model. Figure 2 summarises the results shown in Figure 1(c).
Figure 1: MLP-based diagnostic predictions of 30 neurosurgical cases. The predictions were made using MLP for discerning between lesion or non-lesional (a), glial or non-glial (b), and a summary of the accuracy of predictions made for the four diagnostic categories [1].
Figure 2: Summary of predictive accuracy across tumour classifications (predicted by the utilisation of MLP artificial intelligence technology). Adapted from D. A. Orringer et al., 2017, Rapid intraoperative histology of unprocessed surgical specimens via fibre-lased based stimulated Raman scattering microscopy.
Deep learning (DL) is another form of AI that utilises models based on neural networks to imitate the analytical capabilities of the human brain, particularly in the processing of extensive large data. This approach finds applications in diverse fields, including language processing, image recognition, and drug discovery.
Study 2:
Peritoneal metastasis (PM) is the most common form of distant metastasis and one of the leading causes of death in gastric cancer. Accurate PM diagnosis is clinically significant for treatment and prognosis [3]. In this research, the authors introduced stimulated Raman molecular cytology (SRMC), an intelligent cytology method based on stimulated Raman scattering (SRS) microscopy, for diagnosing PM from gastric cancer. The study utilised single-cell segmentation algorithms based on deep learning to extract 19 features associated with the morphology and composition of individual cells found in ascites. The team used a hybrid algorithm, K-PCA, combining K-means cell clustering and principal component analysis to simplify and transform distinct cell features. This process identified important marker cell groups, and their feature differences were used to differentiate between cases with positive and negative PM. The study incorporated machine learning classifiers, including support vector machine, linear discriminant analysis, and logistic regression to develop a diagnostic model for PM. The model was trained using the feature matrix and the actual PM results as inputs. Adding composition information significantly improved PM detection sensitivity from 59.25% to 81.5%, emphasising the importance of cellular features. Achieving 84.9% specificity in 20 minutes for 80 patients, the SRMC method shows promise for swiftly and accurately detecting PM in gastric cancer with minimal invasiveness.
AI in Healthcare: An Ethical and Social POV
AI stands out as a transformative tool, not as a replacement for the invaluable skills and knowledge of healthcare professionals, but as a means to elevate their capabilities in accuracy and diagnosis. As we enter this transformative phase, societal concerns prompt reflections on the ethical implications of incorporating AI into healthcare. Striking a balance between potential benefits and ethical considerations is vital to align seamlessly with our shared healthcare values.
Training AI algorithms in healthcare can improve outcomes, but it relies on extensive data input. Concerns arise about bias when training data needs to accurately represent the target population, hindering generalisation and potentially overestimating measures for specific racial or societal groups [5]. This bias can lead to unequal treatment in AI algorithms, emphasising the importance of ensuring fairness and mitigating biases. This is crucial to prevent unfavourable outcomes, safeguard patient privacy, and foster trust among patients and healthcare practitioners.
Initially developed for European-descent demographics, AI technologies face challenges in addressing the health concerns of Māori and Pasifika populations in New Zealand [5]. Diverse backgrounds need inclusion in AI datasets to understand health variations across populations. For example, AI algorithms for drug discovery should consider drug effectiveness across diverse populations. Developers must exercise caution concerning dataset variations, unintentional biases, and complexities in generalising to different populations.
Despite the ethical concerns around potential misuse, it is crucial to alleviate existing healthcare disparities with the widespread availability of AI technology. The goal is to harness AI’s potential universally, irrespective of socio-economic circumstances. Specific demographics, such as Māori and Pasifika communities in New Zealand, have faced negative impacts in healthcare. It is essential for AI algorithms not only to include these communities in datasets but also to ensure accessibility and affordability. AI-driven resource allocation systems should prioritise patients based on medical needs rather than financial status. However, international guidelines often overlook the importance of addressing persistent disparities endured by Māori. Aligning these efforts with the principles of Te Tiriti and insights from the Waitangi Tribunal Inquiry into Health Services and Outcomes is imperative [6]. The transformative power of AI in healthcare extends beyond diagnostics, offering a comprehensive approach to personalised care, early disease detection, and ethical considerations. As we navigate this technological evolution, the integration of AI stands as a hope for equitable, accessible, and advanced medical and healthcare solutions [7].
[1] D. A. Orringer et al., “Rapid intraoperative histology of unprocessed surgical specimens via fibre-laser-based stimulated Raman scattering microscopy,” Nature Biomedical Engineering, vol. 1, no. 2, Feb. 2017, doi: 10.1038/s41551-016-0027.
[2] B. Han, S. H, and H. T. Wang, “Machine Learning and AI in Cancer Prognosis, Prediction, and Treatment Selection: A Critical approach,” Journal of Multidisciplinary Healthcare, vol. Volume 16, pp. 1779–1791, Jun. 2023, doi: 10.2147/jmdh.s410301.
[3] 5. S. D. Lee, K. W. Ryu, B. W. Eom, J. H. Lee, M. C. Kook, and Y. W. Kim, “Prognostic significance of peritoneal washing cytology in patients with gastric cancer,” British Journal of Surgery, vol. 99, no. 3, pp. 397–403, Nov. 2011, doi: 10.1002/bjs.7812.
[4] B. Hunter, S. Hindocha, and R. W. Lee, “The role of artificial intelligence in early cancer diagnosis,” Cancers, vol. 14, no. 6, p. 1524, Mar. 2022, doi: 10.3390/cancers14061524.
[5] S. Reddy, S. Allan, S. Coghlan, and P. Cooper, “A governance model for the application of AI in health care,” Journal of the American Medical Informatics Association, vol. 27, no. 3, pp. 491– 497, Nov. 2019, doi: 10.1093/jamia/ocz192.
[6] R. Whittaker et al., “An example of governance for AI in health services from Aotearoa New Zealand,” Npj Digital Medicine, vol. 6, no. 1, Sep. 2023, doi: 10.1038/s41746-023-00882-z.
[7] S. Huang, J. Yang, S. Fong, and Q. Zhao, “Artificial intelligence in cancer diagnosis and prognosis: Opportunities and challenges,” Cancer Letters, vol. 471, pp. 61–71, Feb. 2020, doi: 10.1016/j.canlet.2019.12.007.
Sanchani is completing her BSc, double majoring in Computer Science and Biological Sciences (Genetics). She aspires to combine both areas of her degree by implementing AI and software development solutions to advance genetics and healthcare in this digital age.